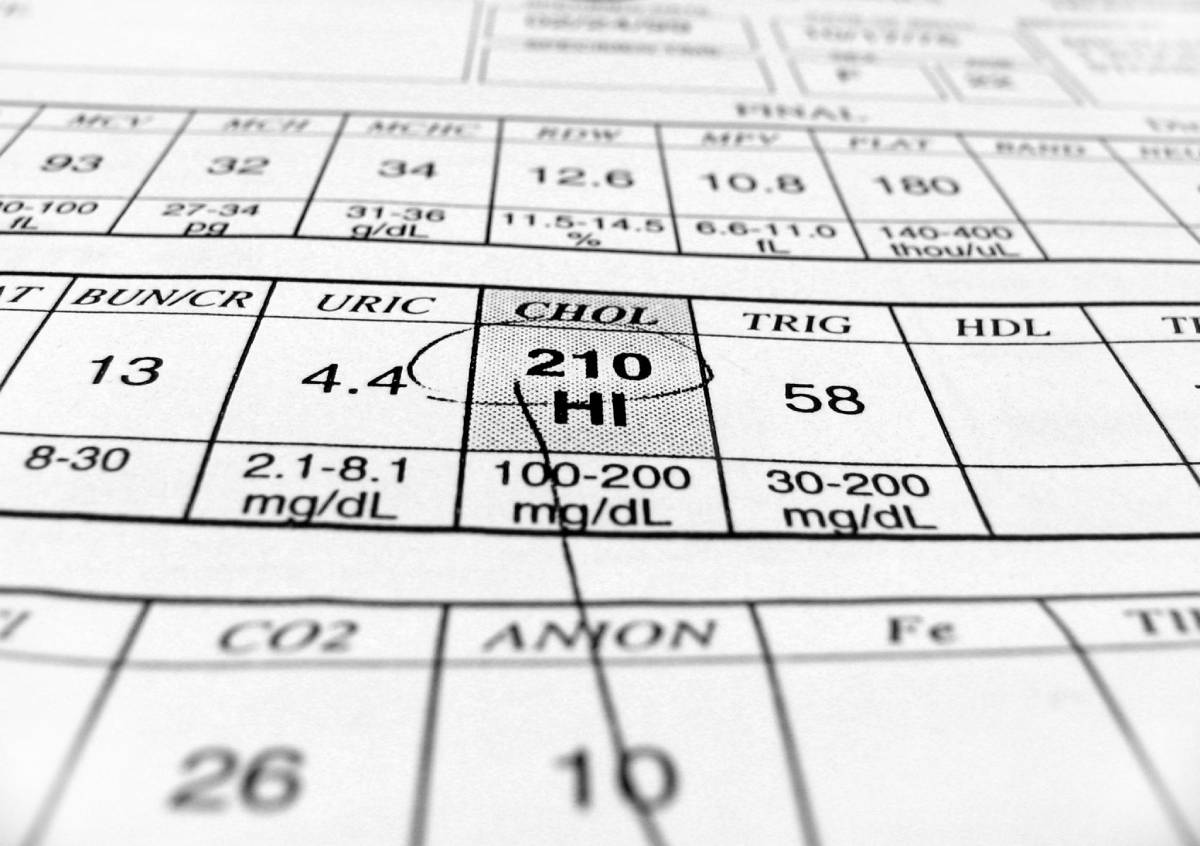
The risks associated with high cholesterol are numerous. Not only can high cholesterol prompt chest pain, but it can also culminate in events as serious as heart attack and stroke. [1] While some researchers have examined how low cholesterol affects the success of operations such as coronary artery bypass grafts and valve replacement [2, 3], an underexamined subject of study is the effect of high cholesterol on surgery outcomes. Accordingly, this article will discuss whether there are any contexts in which high cholesterol impacts surgery outcomes.
The most prominent example of an operation where high cholesterol contributes to poor surgical outcomes is arthroscopic rotator cuff surgery. According to a study presented at the 2017 Annual Meeting of the American Academy of Orthopaedic Surgeons, patients with moderate or high low-density lipoprotein cholesterol (LDL-C) or total cholesterol levels are more likely to require revision rotator cuff surgery in the future [4]. Furthermore, patients who took statins, which are medications used to lower cholesterol levels, before or after surgery did not exhibit higher rates of revision procedures [4]. Regardless of whether their preoperative cholesterol levels were elevated or not, this result held [4].
The beneficial effect of statins on surgical outcomes has been noted in other contexts as well. Beginning in 2007, the American Heart Association and the American College of Cardiology recommended that patients continue using statins before surgery [4, 5]. Patients should also continue taking statins at normal levels and frequency after surgery because those who do not resume statin medication may have a 40% higher risk of two-day mortality, compared to patients who never stopped or promptly resumed taking statins [5]. Although statins lower cholesterol levels, it is important to note that these results may be explained by other attributes of these medications, such as the fact that they promote blood flow and reduce inflammation [5]. Therefore, one cannot take these findings to prove that lowered cholesterol levels promote positive surgery outcomes or, conversely, that high cholesterol negatively impacts outcomes.
Similarly to those who undergo arthroscopic rotator cuff surgery, patients receiving isolated coronary artery bypass grafts may have an increased risk of negative outcomes or complications if they exhibit high LDL-C levels [6]. Lim et al. conducted a retrospective analysis of the cases of 309 consecutive patients who received grafts [6]. They identified elevated LDL-C levels, along with elevated non-high-density lipoprotein cholesterol (HDL-C) levels broadly, as independent predictors of long-term cardiac death [6]. Moreover, the researchers found an association between cardiac death and heightened LDL-C, non-HDL-C, and total cholesterol (TC) levels, as well as TC/HDL-C ratio [6].
High cholesterol may result in postoperative visual loss (POVL) following non-ocular surgeries [7]. A groundbreaking population-based study conducted by Northwestern Medicine found that patients undergoing orthopedic or cardiac surgeries were more likely to wake up blind after their operations if they have high cholesterol levels [7]. This is perhaps the most generalizable result so far identified in the scientific literature analyzing high cholesterol and surgical outcomes.
All in all, the connection between high cholesterol and surgery outcomes is not altogether clear. While convincing evidence may connect high cholesterol with adverse outcomes following arthroscopic rotator cuff surgery and coronary artery bypass grafts, even in these cases, more research is necessary to determine the accuracy of these results and whether there is any causality to the relationship.
References
[1] Mayo Clinic, “High cholesterol,” Updated July 20, 2021. [Online]. Available: https://www.mayoclinic.org/diseases-conditions/high-blood-cholesterol/symptoms-causes/syc-20350800.
[2] Y.-L. Lee et al., “Body mass index and cholesterol level predict surgical outcome in patients with hepatocellular carcinoma in Taiwan – a cohort study,” Oncotarget, vol. 7, no. 19, p. 22948-22959, March 2016. [Online]. Available: https://doi.org/10.18632%2Foncotarget.8312.
[3] H.-B. Li et al., “Low-Density Lipoprotein Cholesterol and Mortality Risk in Elderly Patients Undergoing Valve Replacement Surgery: A Propensity Score Matching Analysis,” Frontiers in Nutrition, vol. 9, p. 1-8, April 2022. [Online]. Available: https://doi.org/10.3389/fnut.2022.842734.
[4] American Academy of Orthopaedic Surgeons, “Statins use prior to surgery mitigates risk,” Science Daily, Updated March 14, 2017. [Online]. Available: https://www.sciencedaily.com/releases/2017/03/170314081630.htm.
[5] American Society of Anesthesiologists, “Surgical patients should stay on cholesterol medications to reduce risk of death, study shows,” Updated October 27, 2015. [Online]. Available: https://www.asahq.org/about-asa/newsroom/news-releases/2015/10/surgical-patients-should-stay-on-cholesterol-medications.
[6] K. Lim et al., “Influence of cholesterol level on long-term survival and cardiac events after surgical coronary revascularization,” JTCVS Open, vol. 10, p. 195-203, June 2022. [Online]. Available: https://doi.org/10.1016/j.xjon.2022.02.022.
[7] J. C. Lin et al., “Epidemiology of postoperative visual loss for non-ocular surgery in a cohort of inpatients,” Eye, vol. 36, p. 1323-1325, November 2021. [Online]. Available: http://dx.doi.org/10.1038/s41433-021-01791-9.