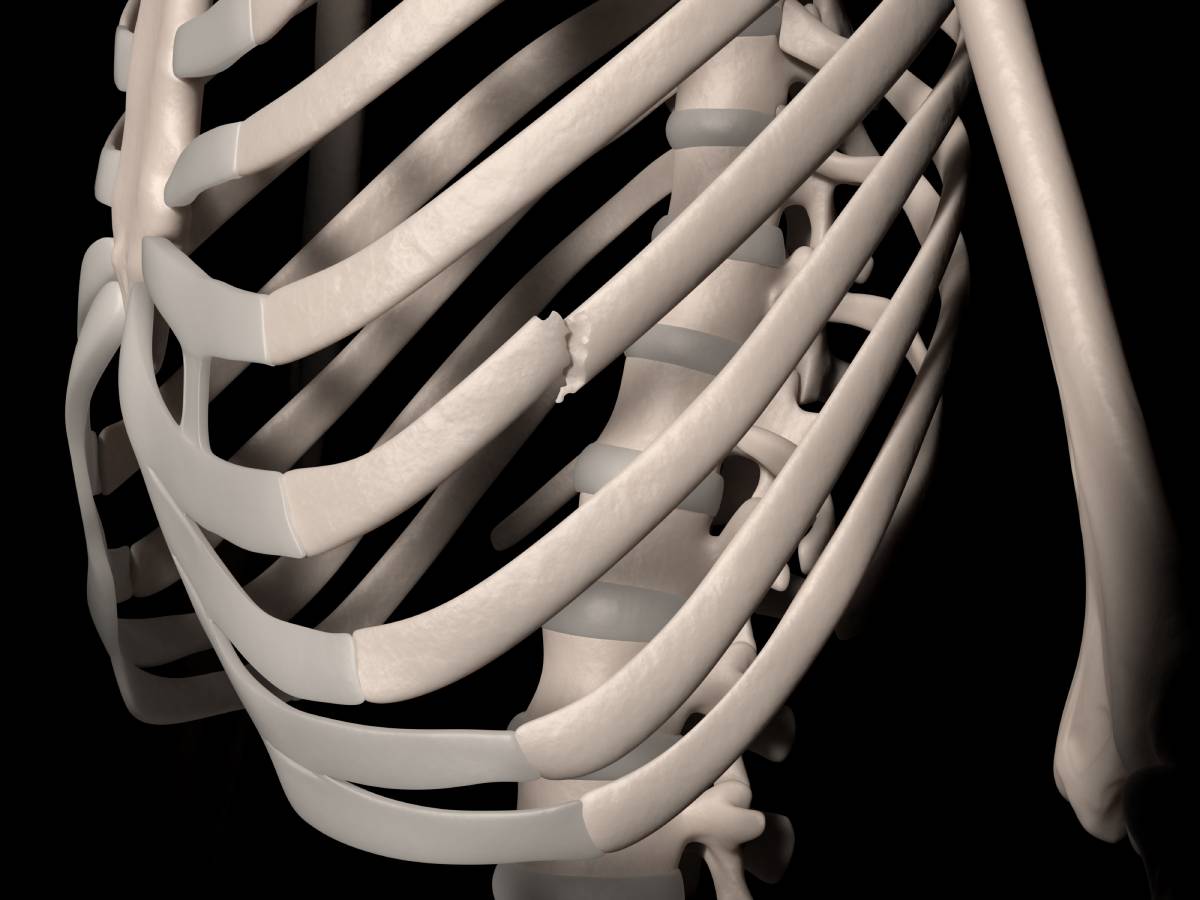
Rib fractures often occur following thoracic trauma—approximately 10% of patients after blunt chest trauma suffer one or more rib fractures 2—and are associated with significant morbidity and mortality 1. Simple rib fractures are the most frequent injury following blunt chest trauma, resulting from over half of thoracic injuries from nonpenetrating trauma. Though broken ribs do often do not require surgery, they can be painful, and anesthesia may be needed in some cases to provide relief. Several pain relief options have been established for relief from rib fracture pain 3.
Thoracic epidural analgesia is an effective regional anesthesia technique for broken ribs, in particular when injuries are bilateral. Research has shown that epidural analgesia may improve clinically significant outcomes and should be considered the preferred analgesic modality.
Several studies have validated the effect of thoracic epidural analgesia on outcomes. One study sought to assess patients receiving either thoracic epidural analgesia with bupivacaine or intravenous opioid therapy 4. The relative risk of pneumonia in the opioid group was found to be 6-fold higher. In addition, the epidural analgesia group had about half the number of days requiring mechanical ventilation, as has been confirmed by a number of other studies.
As compared with intravenous opioids or intrapleural bupivacaine, thoracic epidural analgesia also reduces the pain associated with coughing or deep breathing. A retrospective review demonstrated that while thoracic epidural analgesia provided superior analgesia to intravenous patient-controlled morphine, the length of stay in the hospital or intensive care unit, as well as major morbidity, remained unaffected. Another meta-analysis failed to show a difference in major outcomes such as mortality, hospital or intensive care unit length of stay, and duration of mechanical ventilation with epidural analgesia.
Although thoracic epidural analgesia is effective at reducing morbidity and other outcomes following rib fractures, it is not appropriate for all patients. Contraindications include hypotension and hypovolemia, coagulopathy, spinal or head injury, and sepsis.
Paravertebral nerve block is an alternative regional anesthesia procedure that provides excellent unilateral or bilateral analgesia for broken ribs. A catheter technique is typically used for fractured ribs. Following insertion, the block can be increased through the administration of more anesthetic.
Thoracic epidural analgesia and thoracic paravertebral nerve block methods have been found to be equivalent with respect to pain relief, the incidence of pulmonary complications, and improvement in respiratory function. Though minor, risks include contralateral spread via the epidural space, pneumothorax, vascular puncture, and hypotension.
An advantage of a paravertebral nerve block catheter is its capacity for long-term analgesia in an ambulatory context. The case of a patient with multiple unilateral rib fractures who was experiencing intense pain and respiratory distress was reported in the literature 5, in which a paravertebral catheter successfully provided rapid and long-lasting relief. Another report documented an anesthesiology resident experiencing debilitating pain from multiple fractured ribs who was able to carry on with clinical work for 18 days, opioid-free, while receiving an infusion of local anesthetic through a paravertebral catheter 6.
Alternative regional techniques have also been used to provide anesthesia for broken ribs. Intercostal blocks provide strong initial relief but remain limited in their duration of action. In addition, the risk of pneumothorax remains substantial. Intrapleural block with local anesthetic is also limited in efficacy and incurs the risk of the local anesthetic being rapidly absorbed systemically. Finally, transdermal lidocaine patches placed over rib fracture sites have not yet been shown to substantially improve pain in patients suffering from rib fractures.
There are clear benefits and drawbacks to different anesthetic techniques for rib fractures. It remains critical, according to the clinical context, to select the best method based on the patient’s background and preferences.
References
1. Peek, J. et al. Epidemiology and outcome of rib fractures: a nationwide study in the Netherlands. Eur. J. Trauma Emerg. Surg. (2022). doi:10.1007/s00068-020-01412-2
2. Kasotakis, G. et al. Operative fixation of rib fractures after blunt trauma: A practice management guideline from the Eastern Association for the Surgery of Trauma. in Journal of Trauma and Acute Care Surgery (2017). doi:10.1097/TA.0000000000001350
3. Regional Anesthesia in Patients with Trauma – NYSORA | NYSORA. Available at: https://www.nysora.com/topics/sub-specialties/trauma/regional-anesthesia-patients-trauma/. (Accessed: 23rd May 2023)
4. Berger, A., Tizian, C. & Zenz, M. Continuous plexus blockade for improved circulation in microvascular surgery. Ann. Plast. Surg. (1985). doi:10.1097/00000637-198501000-00004
5. Murata, H., Salviz, E. A., Chen, S., Vandepitte, C. & Hadzic, A. Ultrasound-guided continuous thoracic paravertebral block for outpatient acute pain management of multilevel unilateral rib fractures. Anesth. Analg. (2013). doi:10.1213/ANE.0b013e31826f5e25
6. Buckley, M., Edwards, H., Buckenmaier, C. C. & Plunkett, A. R. Continuous thoracic paravertebral nerve block in a working anesthesia resident-when opioids are not an option. Mil. Med. (2011). doi:10.7205/MILMED-D-10-00413